SNRI Drugs (Serotonin-norepinephrine reuptake inhibitors) act primarily upon serotonergic and noradrenergic neurons but have little or no effect upon cholinergic or histaminergic receptors. SNRI drugs are primarily used to treat patients with major depression, however, they are also utilized in the treatment of fibromyalgia.
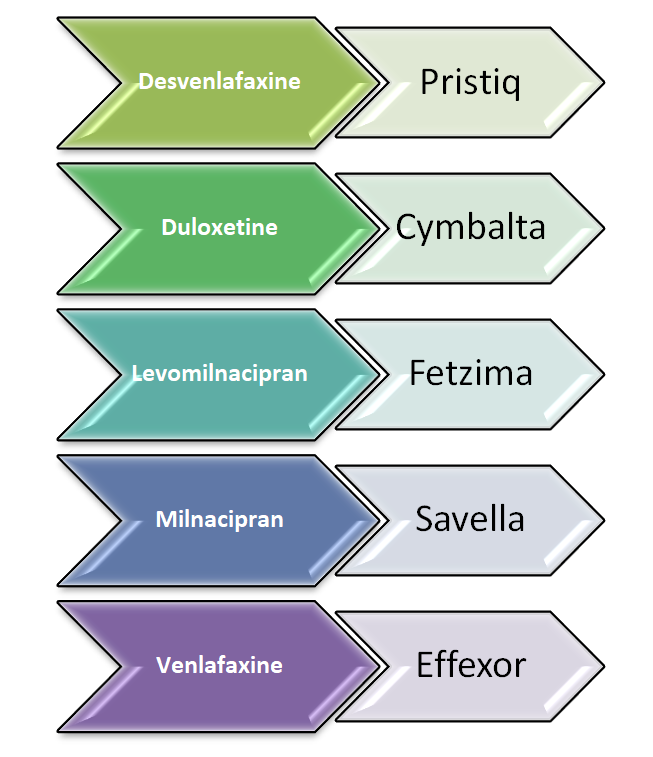
SNRI drugs include:
- Desvenlafaxine
- Duloxetine
- Levomilnacipran
- Milnacipran
- Venlafaxine
Generic and Brand Names of various SNRI Drugs:
SNRI Drugs (Serotonin Norepinephrine Reuptake Inhibitors) are used to treat the following disorders:
- Depressive disorders (eg unipolar major depression or persistent depressive disorder also called dysthymia,
- Anxiety disorders e.g. generalized anxiety disorder (GAD), panic disorder or social anxiety disorder,
- Chronic pain syndromes like fibromyalgia or diabetic peripheral neuropathy,
- Obsessive-compulsive disorder,
- Body dysmorphic disorder, and
- Posttraumatic stress disorder,
- Menopausal hot flushes,
- Vulvodynia and
- Urinary incontinence
What are SNRI Drugs and how do they act?
Structure of SNRI Drugs:
- Desvenlafaxine (also called O-desmethylvenlafaxine) and venlafaxine are bicyclic phenylethylamine compounds that have got similar structures. There is a slight difference between Venlafaxine and desvenlafaxine. The removal of a methyl group from venlafaxine results in the active metabolite desvenlafaxine.
- Duloxetine is a naphthalene compound.
- Milnacipran, a phenylacetamide compound, consists of two stereoisomers. They are mirror images of one another and cannot be superimposed on each other (similar to one’s hands). One of the stereoisomers is Levomilnacipran. It is the active drug and enantiomer of racemic milnacipran.
- Although the mechanism of action of SNRIs is identical, the structures of duloxetine and milnacipran are different.
How SNRI Drugs Act?
- The SNRIs are thought to be effective in treating depression by blocking presynaptic and norepinephrine transporter protein. This prevents reuptake and alters many homeostatic mechanisms. It increases stimulation of postsynaptic receptors. The SNRIs have different affinity for serotonin transporter, and norepinephrine transporter.
- Desvenlafaxine, duloxetine, and norepinephrine are stronger inhibitors for serotonin uptake. Levomilnacipran and milnacipran preferentially inhibit the reuptake of norepinephrine.
Since SNRI inhibit the reuptake of Serotonin and nor-epinephrine, they are called the “dual-action agent”
The degree of SNRIs on the serotonin vs norepinephrine is dependent on the dose that is administered.
- Venlafaxine is a selective serotonin reuptake inhibitor (SSRI) at 75 mg daily. Venlafaxine can have significant effects on norepinephrine transporter at higher doses (e.g. 225 mg/day or 375 mg/day).
- Levomilnacipran blocks norepinephrine transporter approximately twice as well as serotonin even at low doses. Levomilnacipran doses greater than 40 mg per day block 90 percent of norepinephrine and 80 percent serotonin reuptake, respectively.
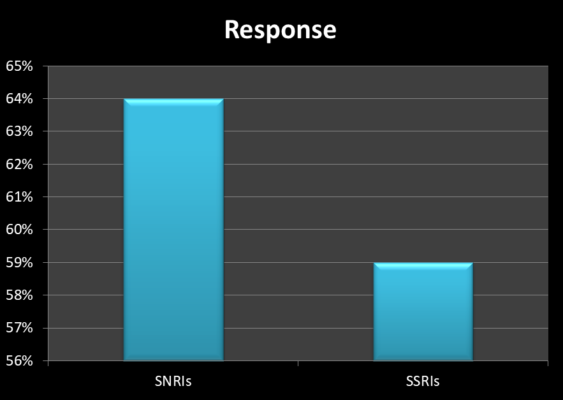
Drugs that block serotonin-norepinephrine reuptake are more effective than SSRIs for treating major depressive disorder. The benefit is however modest. The pooled analysis of 93 randomized trials with more than 17,000 patients showed that dual-action drugs had a greater response rate (64 versus 59%). Although the difference was statistically significant, the magnitude of the effect was small [Ref].
The SNRIs do not have any effect on alpha1-adrenergic or cholinergic receptors. However, SNRIs stimulate norepinephrine receptors in the sympathetic nervous system, which leads to a relative decrease in parasympathetic tone; this can cause “pseudo-anticholinergic” side effects such as constipation, dry mouth, and urinary retention, despite the lack of direct effects upon cholinergic receptors. Because of its anticholinergic effects, it is also used to treat urinary incontinence.
Pharmacokinetics of SNRI Drugs:
The rate of absorption of SNRI Drugs is affected by food. SNRIs can cause nausea that can also affect food intake and the drug’s absorption. Duloxetine is protein-bound and is primarily excreted via the liver.
On the other hand, other SNRIs are less protein-bound. Drug clearance is influenced more by kidney excretion. Patients with kidney disease are more likely to have the drug excreted unchanged from their urine.
Levomilnacipran is only 22 percent bound to plasma proteins, and 58 percent are excreted unchanged from the urine. Due to interindividual differences, steady-state plasma concentrations may differ between individuals due to variations in clearance. Individual dose adjustments may be required to achieve the desired clinical effect. Patients suffering from liver or kidney disease will need to be prescribed a lower dose.
Drug-drug interactions:
Duloxetine is a moderately potent inhibitor of the hepatic cytochrome P450 enzyme CYP2D6 and may interact with other drugs. Clinically, there are no significant clinical effects of desvenlafaxine, milnacipran, or levomilnacipran on the P450 enzymes.
Patients who have taken monoamine oxidase inhibitors (MAOIs) in the last two weeks should not take SNRIs. Because drug-drug interactions may lead to serotonin syndrome and hypertensive crises, this is important. Patients should wait at least two weeks before stopping SNRIs and starting MAOIs.
General Principles of treatment using SNRI Drugs:
Before initiating the treatment, educate the patient about the effects and side effects of the drugs. Patients should be aware that although some symptoms can be seen in two weeks, recovery can take between eight and twelve weeks. How quickly depressed patients respond can depend on the severity of their illness, comorbidities, and other factors.
Clinicians should warn patients not to abruptly stop taking SNRIs. This could cause withdrawal symptoms or discontinuation syndrome such as dizziness, dizziness and dysphoria, fatigue, and gastrointestinal distress. This discontinuation syndrome is more common for venlafaxine than for milnacipran.
SNRIs have been linked to an increase in blood pressure. It is important to monitor your blood pressure throughout any SNRI treatment. You should adjust your antihypertensive medication if your blood pressure is too high before you start treatment. Alternate antidepressants might also be recommended. Patients who are taking SNRIs should have their blood pressure checked at least once per month. Then, it is checked every one to six month thereafter. The monitoring continues every three to six months thereafter. The SNRI and dose may affect the schedule.
Venlafaxine at a low doses has a minimal effect on blood pressure.
Dosage of SNRI drugs:
The dose and duration of the treatment with SNRI drugs are variable and dependent solely on the patient’s condition and comorbid disease state. To prevent side effects, start SNRIs with a low dose. Gradually increase the dose until you get the desired clinical response. The indication will determine the maximum dose, starting dose, and titration plan. Patients suffering from anxiety disorders or depression might be able to tolerate half of the recommended dose. Doses are adjusted according to patient response, tolerance, clinical urgency, and clinical urgency.
The key to finding the right antidepressant dose is trial and error. Start the antidepressant and increase the dosage to the recommended minimum dose. Monitoring the patient’s reaction over the next 2 to 4 weeks is important. Patients who cannot tolerate the drug are allowed to increase their dose. Patients who show improvement are given more time.
Venlafaxine, the most widely studied SNRI (fixed-dose random trials), shows that higher doses of venlafaxine have a greater effect on unipolar major depression disorder. A dose-response meta analysis of venlafaxine included 10 fixed-dose random trials lasting 6-12 weeks with 16 treatment groups. To reduce baseline symptoms 50 percent, the dose of venlafaxine increased from 75 mg to 150 mg/day. Doses above 375 mg/day saw a modest increase in response. Patients stopped taking venlafaxine for adverse effects at an increasing rate. This suggests that the lowest therapeutic dose might be the most effective in balancing tolerance and response [Ref].
Side effects of SNRI Drugs:
The most common side effects of SNRIs include:
- Nausea
- Dizziness
- Excessive sweating
Side effects, especially nausea appear to diminish over time.
Here are some other side effects:
- An increase in Blood pressure:
- Blood pressure may increase due to the drug’s effects on norepinephrine. Sustained and persistent hypertension is rarely seen.
- Headaches:
- Headaches can be common during antidepressant trials but also in patients with depression before treatment or who were given placebo.
- Sexual dysfunction:
- SNRIs report moderate levels of sexual dysfunction (erectile dysfunction and delayed ejaculation). However, sexual impairment rates that are spontaneously reported are often lower than those that have already been systematically assessed.
Read: Sertraline and Erectile Dysfunction (Zoloft effect on ED)
- Bleeding and effect on bone resorption:
- SNRIs block serotonin reuptake by platelets and osteocytes. Although there are not many reports, SNRIs have been linked to increased bleeding risk and bone resorption.
- Although the risk is minimal, patients already receiving anticoagulants should be more cautious. Likewise, patients with pre-existing osteoporosis may be at an increased risk of fractures.
- Hyponatremia:
- SNRIs seem to be associated with hyponatremia in older patients (eg, >65 years), who are taking diuretics or have a history of hyponatremia. Hyponatremia increases the risks of falls, cognitive dysfunction, osteoporosis, posture instability, and is associated with higher morbidity or mortality.
- It is generally thought that SNRIs have little effect on serum sodium levels compared to SSRIs. However, since hyponatremia can be serious, patients at risk of hyponatremia should be cautious and monitor serum sodium levels at regular intervals.
- Stress Cardiomyopathy:
- There is evidence that stress cardiomyopathy may be related to SNRIs. However, this has not been proved causal.
- Suicide:
- All SSRIs and SNRIs have been associated with an increased risk of suicidal tendencies especially in younger age groups such as those aged less than 18 years of age.
- Patients and the caregivers are asked to report any new-onset behavioral changes that could be indicative of an increased risk of suicidal tendency.
In conclusion:
Serotonin-norepinephrine reuptake inhibitors (SNRIs) include desvenlafaxine, duloxetine, levomilnacipran, milnacipran, and venlafaxine. SNRIs can be efficacious for treating unipolar major depression. These drugs act by blocking the uptake of serotonin and norepinephrine at the synaptic terminals.
Except for Duloxetine, SNRIs have minimal drug-drug interactions. Treatment with SNRIs is usually initiated in low doses and then gradually titrated upwards until clinical response is achieved or the target dose is reached. With increasing doses, side effects may result. The most common side effect of SNRIs is nausea. Other side effects include dizziness, constipation and dry mouth.
SNRIs can also have effects on the blood pressure. Like SSRIs, these drugs can cause some degree of sexual dysfunction too. When used for a prolonged period of time, it can result in weight gain (of up to 5 kgs). Additionally, SNRIs can increase the risk of bleeding, bone loss, and cause hyponatremia.
Abrupt discontinuation of SNRIs may cause discontinuation symptoms. It is recommended to tape these medications before discontinuing them. While levomilnacipran or milnacipran are less likely than other SNRIs to cause discontinuation symptoms, it is still recommended that you taper if time allows.
Venlafaxine may perhaps be more lethal in overdose than SSRIs.